
Sudocrem® for Pressure Sores

There are several reasons why our mobility can be restricted and, unfortunately, staying in one position for too long can lead to the unwanted result of pressure sores. Regularly checking the skin and changing positions can help prevent it, but once they occur, they can be painful and difficult to treat. Sudocrem®’s versatility means it can relieve the symptoms and and treat the sores.
How Sudocrem®Antiseptic Healing Cream helps pressure sores:

- Contains antiseptic properties helping to reduce the risk of infection
- Maintains hydration to promote tissue repair
- Forms a protective barrier, reducing friction and pressure on the skin
- Contains mild pain relief to help to alleviate discomfort
How to use Sudocrem® on pressure sores:

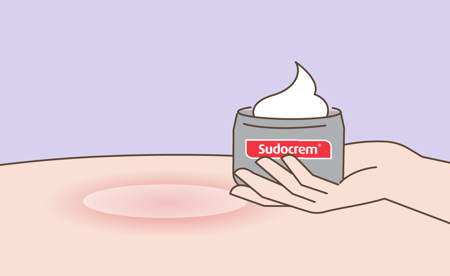
1. Apply
Use small circular movements to create a thin translucent layer

2. Avoid
Rubbing as this may aggravate it further and break the skin
3. Repeat
Use as often as required, but remember – a little goes a long way






